Everything You Need to Know About Top Surgery: Gender-Affirming Chest Reconstruction and Breast Reduction
Medically reviewed by Dr. Scott Mosser on March 13, 2024.
Finally, a group of expert top surgeons inclusive of all identities and body types, with a highly successful insurance concierge.
On This Page
What is gender affirming top surgery?
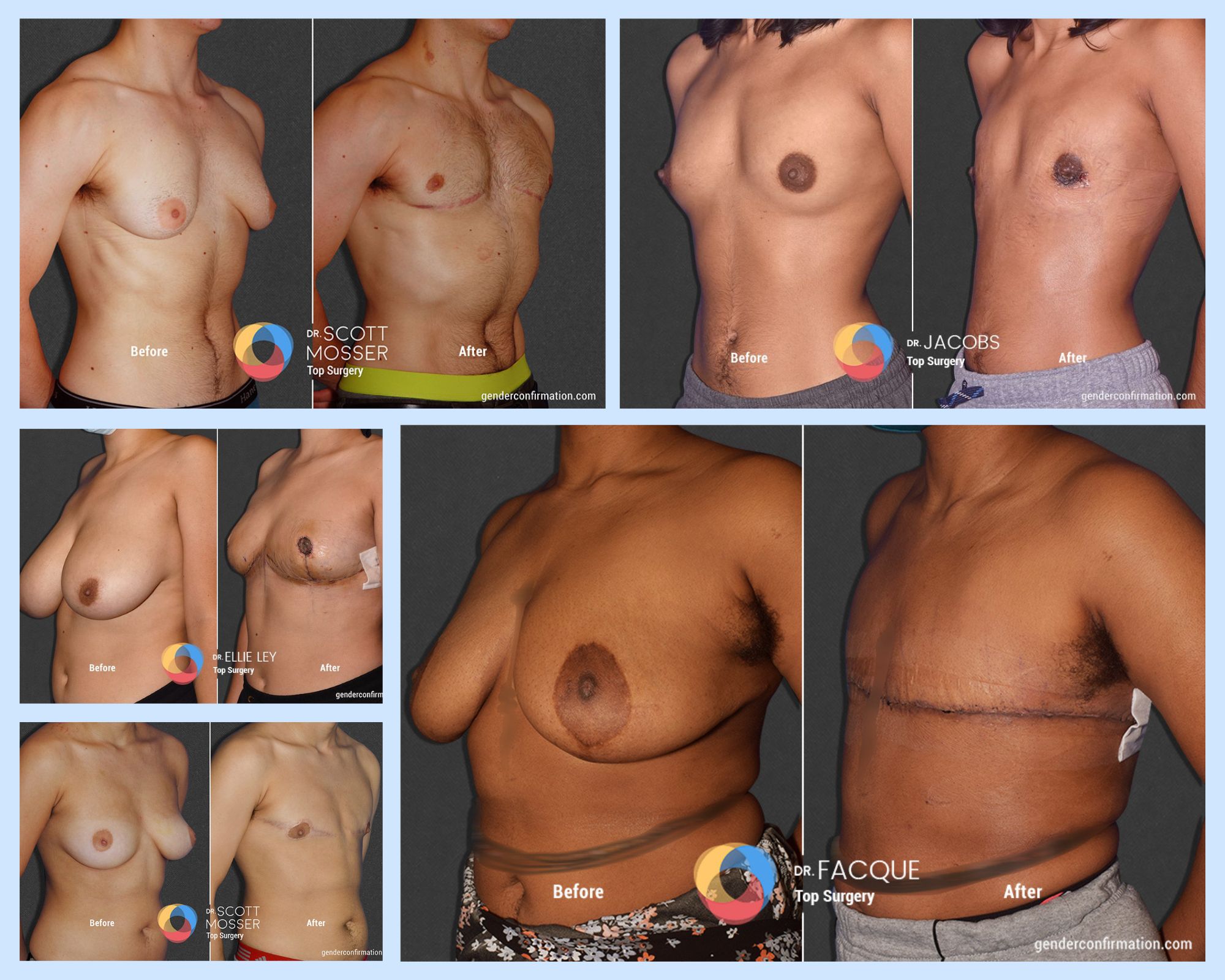
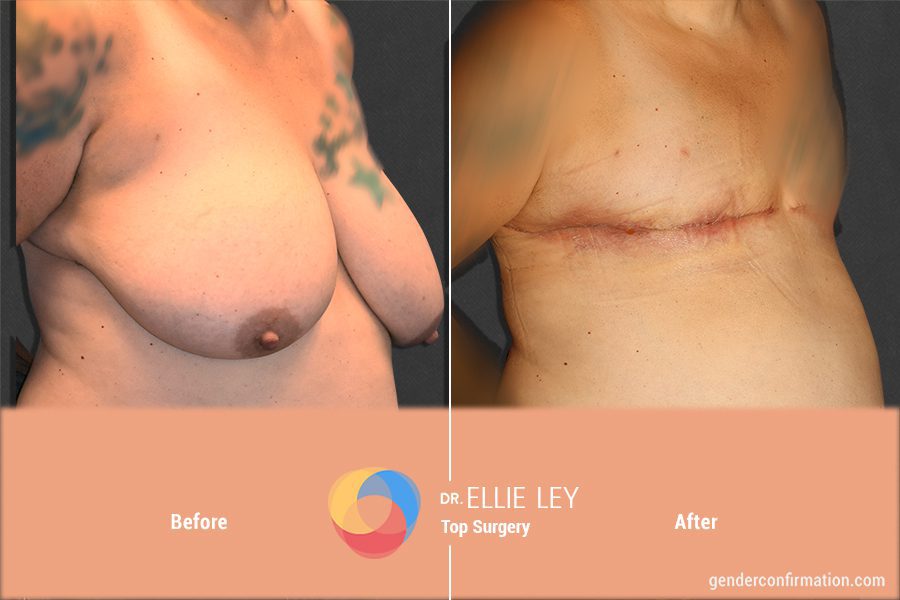
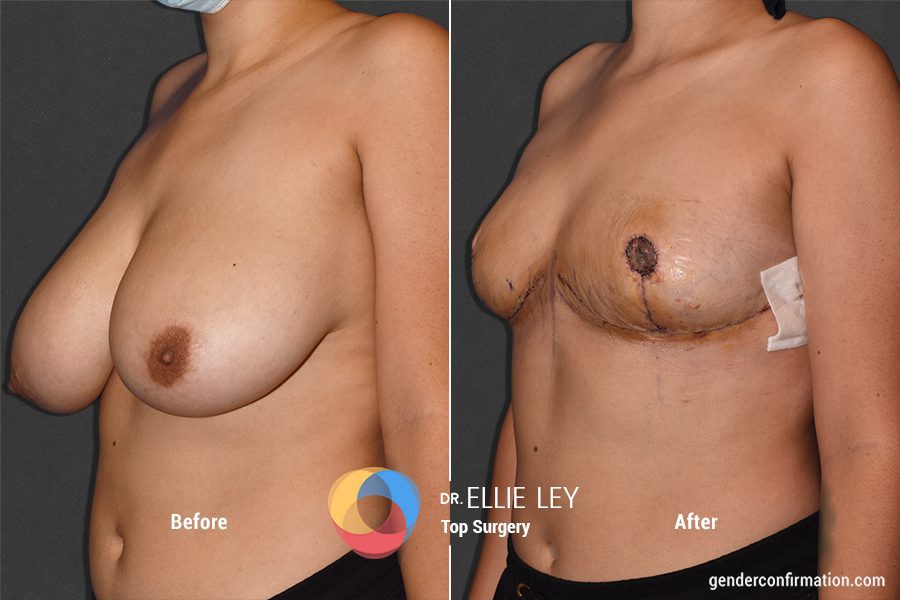
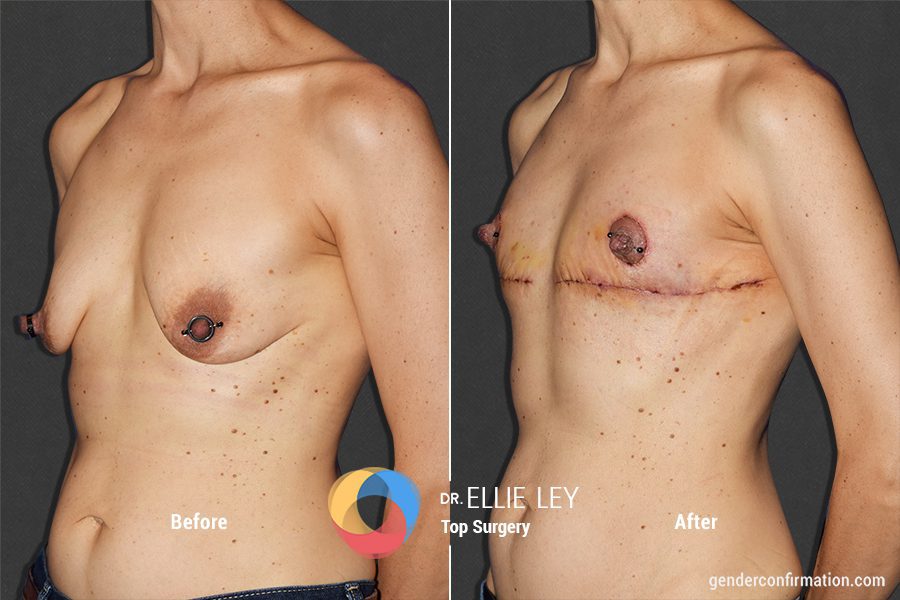
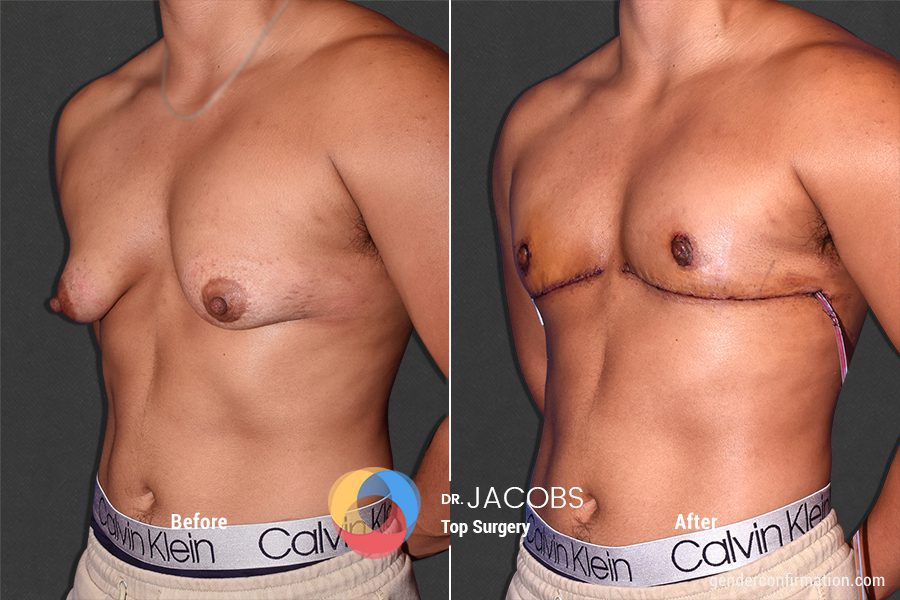
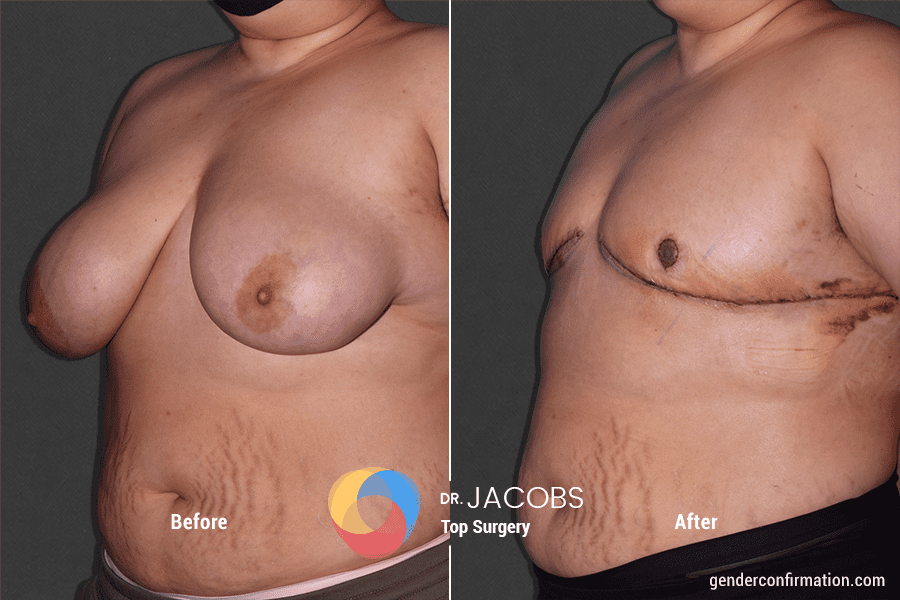
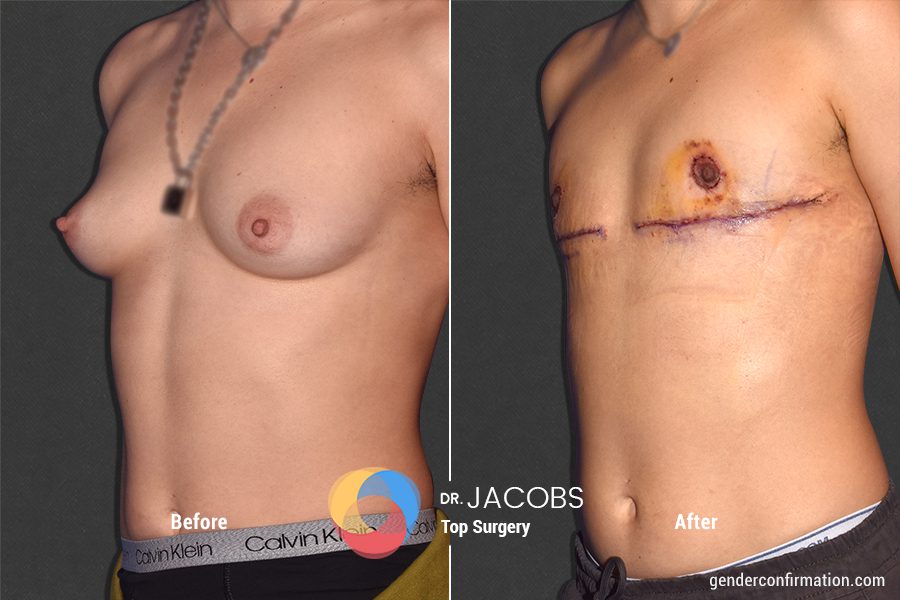
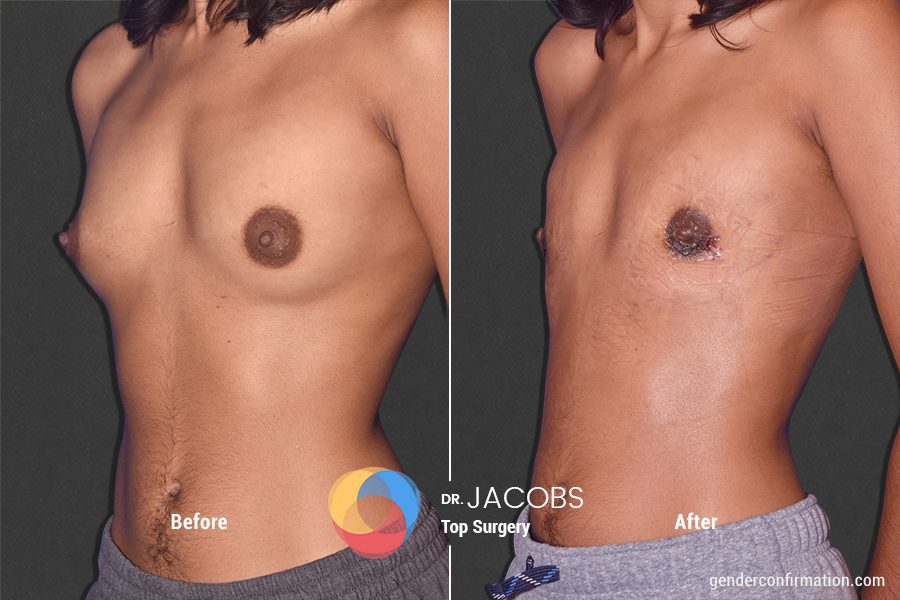
Our board-certified top surgeons + Before & after results
The roadmap to top surgery: how to get and prepare for your operation
Your options considered: What top surgery techniques are available?
-
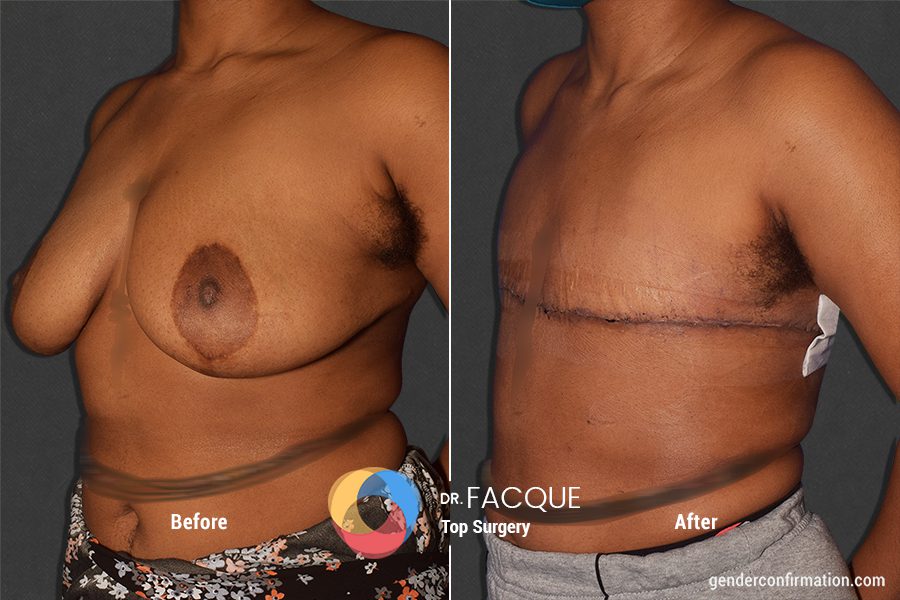
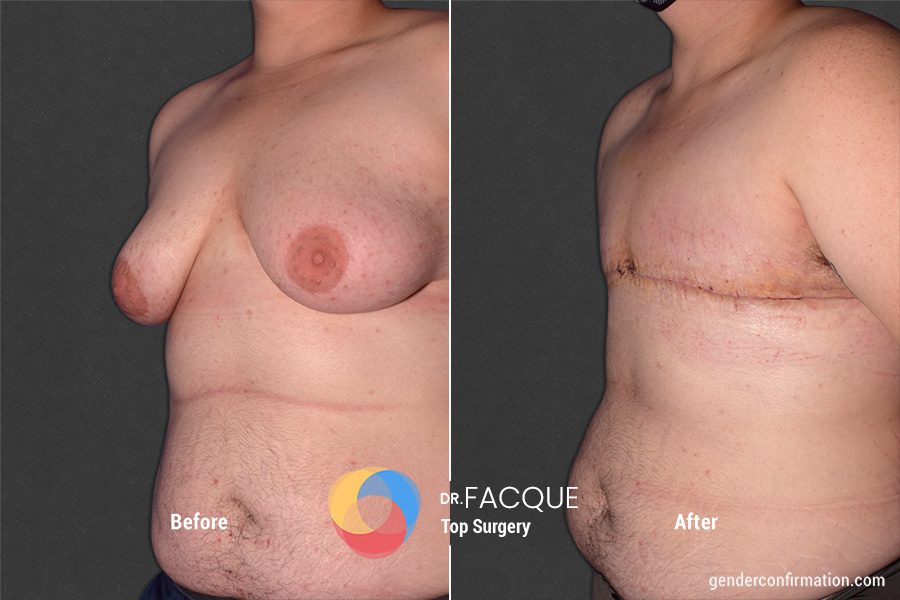
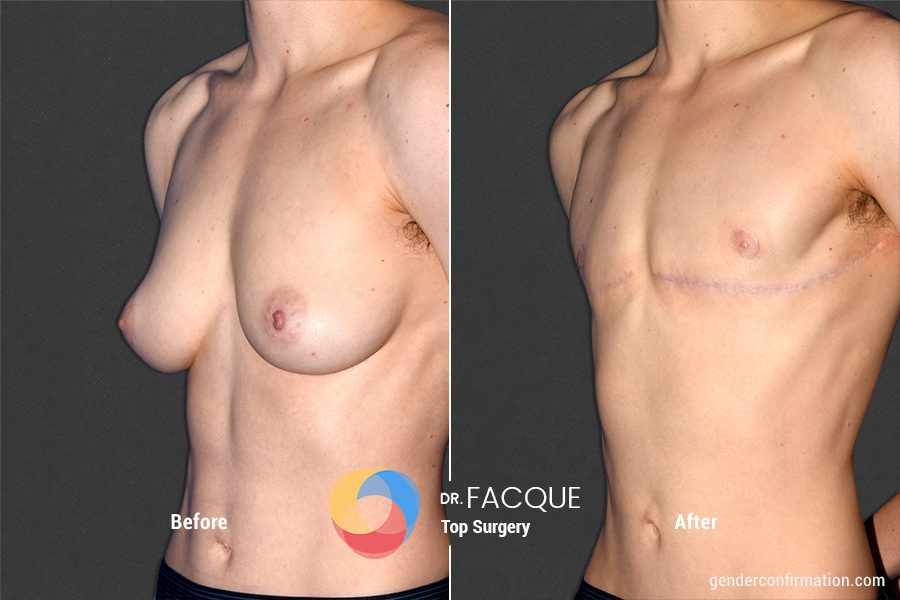
 Dr. Alexander Facque (he/him)
Dr. Alexander Facque (he/him) -
Dr. Alexander Facque (he/him) is a board-certified plastic surgeon and proud member of the LGBTQ+ community. Dr. Facque got his start in gender-affirming care as a resident at the Icahn School of Medicine at the Mount Sinai Medical Center in New York, where he first recognized the importance of providing safe and accessible surgeries to trans and non-binary patients. He then spent a year training and expanding his knowledge under Dr. Loren Schechter, one of the world’s foremost gender-affirming surgeons, as a fellow at Weiss Memorial Hospital’s Gender Confirmation Surgery and Practice Leadership in Chicago. Dr. Facque officially joined our team in 2020 and brought with him over 5 years of previous experience in gender affirming care.
-
 Dr. Ellie Zara Ley (she/her/they)
Dr. Ellie Zara Ley (she/her/they) -
Dr. Ellie Zara Ley (she/her/they) is a board-certified plastic surgeon and the only transgender woman of color to offer a full-spectrum specialization in gender affirming surgery: top surgery, bottom surgery, facial surgery and body contouring. She also specializes transgender adolescent care. She is highly trained, having completing her general surgery residency at University of Arizona, a fellowship in plastic and reconstructive surgery at the University of Utah, a fellowships in craniofacial and pediatric plastic surgery at Primary Children’s Hospital in Salt Lake City and another in hand surgery and microsurgery at the University of Southern California. Prior to joining our team in 2022, she worked as an assistant clinical instructor of plastic surgery at the University of Utah and had her own private practice in Arizona.
-
 Dr. Daniel Jacobs (he/him)
Dr. Daniel Jacobs (he/him) -
Dr. Daniel Jacobs (he/him) brings over 30 years of experience in reconstructive plastic surgery and research. He completed a General Surgery residency at LAC/USC School of Medicine and a Plastic Surgery residency at USC School of Medicine. His exceptional work has been recognized through prestigious medical awards such as the ‘Sidney R. Garfield, MD Exceptional Contribution Award’ in 2017, San Jose Kaiser Permanente’s ‘Outstanding Inpatient Physician of the Year’ in 2017, and the ‘Outstanding Achievement in Medicine’ award from Santa Clara Medical Association in 2016.
-
 Dr. Scott Mosser (he/him)
Dr. Scott Mosser (he/him) -
Dr. Scott Mosser (he/him) is a board-certified plastic surgeon who has over 15 years of experience serving gender diverse patients. He has devoted himself exclusively to gender affirming care since founding the GCC in 2013. Dr. Mosser is also a cofounder of the American Society of Gender Surgeons (ASGS), a member of the American Society of Plastic Surgeons (ASPS), the World Professional Association of Transgender Health, (WPATH), the United States Professional Association of Transgender Health (USPATH), and is a Fellow of the American College of Surgeons (FACS).
To get started on your top surgery journey, you can request a free, virtual consultation with one of our world-class surgeons today.
A consultation is your place to get all of your specific questions about surgery answered by the expert. You can create a unique surgical plan based on your goals, body type and medical history.
There is a lot that goes into preparing for top surgery, which can make it confusing and even overwhelming for some. The information below is meant to help guide you on the steps most patients go through in order to schedule their surgery date. Once you have your surgery date, you can also consult this guide to find content on how to prepare for your operation.
-
 What are the steps involved in getting top surgery?
What are the steps involved in getting top surgery? -
From requesting a consultation, to obtaining insurance approval and completing all other preoperative requirements, we have you covered with our top surgery timeline guide.
-
 Will my insurance cover top surgery?
Will my insurance cover top surgery? -
At the GCC, you can leave the insurance worries to us. We provide an insurance concierge service to interested patients. After soliciting any necessary documents from you, our insurance advocacy team will get to work to secure full or partial coverage for your medically necessary, gender affirming procedure(s). Our team has a 90% success rate in securing coverage for insured patients. Learn more about that process here.
-
 How can I finance my surgery if it’s not covered or only partially covered by insurance?
How can I finance my surgery if it’s not covered or only partially covered by insurance? -
We have compiled a list of scholarships for gender affirming surgeries alongside trusted, medical credit agencies you can use to help finance your surgery with us. You can also find estimated costs for each procedure we offer if you plan on paying entirely out of pocket. Click here for more.
-
 Do I need a letter of approval from a therapist, psychiatrist or primary care doctor to get top surgery with GCC?
Do I need a letter of approval from a therapist, psychiatrist or primary care doctor to get top surgery with GCC? -
Letters of support or clearance letters from certified, mental health professionals are welcome and valuable, but not a requirement for adults who seek surgery with the GCC. This is because we use the informed consent model, which means that a letter from a therapist is not required unless the patient is seeking insurance approval.
Insurance companies always require a letter of support from a mental health professional for approval. If our reconstructive surgeons are outside of your provider network, you will also need a reference letter from your primary care provider to request insurance coverage. For more information, click here.
-
 What about patients who are traveling from out of town to San Francisco for surgery?
What about patients who are traveling from out of town to San Francisco for surgery? -
Many trans, non-binary and gender expansive patients need to travel to access quality, reliable gender affirming surgical care. At the GCC, we are very accustomed to working with patients from out of town. We have compiled a guide on preoperative consultations and post-operative follow-up protocols for patients who do not live in the San Francisco Bay Area. For recommendations on travel and lodging, click here.
-
 Do I need to be taking testosterone hormone replacement therapy to get top surgery?
Do I need to be taking testosterone hormone replacement therapy to get top surgery? -
Taking testosterone is not required before undergoing top surgery. At the GCC, we are committed to serving patients of all gender identities. We believe in taking an individualized approach with each patient to design surgery to meet their unique goals. If you have questions about how testosterone might impact top surgery results, click here.
-
 Results: what will my chest look like after top surgery (mastectomy or breast reduction)?
Results: what will my chest look like after top surgery (mastectomy or breast reduction)? -
One of the most common inquiries we receive from patients is about what their final results will look like. Surgical recovery is a long process that may require patience. This is because final results are not visible until one year after the operation due primarily to inflammation from healing. It is impossible to guarantee what your chest will look like after surgery since everyone heals differently. Still, bringing pictures to your consultation that represent your desired results can help your surgeon decide which techniques would be best suited for you. You can read more about factors that affect the final outcome of a breast reduction or chest reconstruction here.
-
 What options exist for non-binary and gender expansive patients seeking top surgery?
What options exist for non-binary and gender expansive patients seeking top surgery? -
Non-binary and gender expansive are two names for gender identities that transcend or do not fixate on only one of the two binary genders: male or female. At GCC, we recognize that there is no one way to “look non-binary,” just as there is no single, correct way to “look like a woman or man.”
That said, due to our high-volume of non binary patients, we have developed a series of top surgery techniques that respond to the interests commonly expressed by this group. Our approach is based on agreeing with a patient on the most suitable techniques to help them achieve their aesthetic goals and put them at the smallest risk possible for medical complications.
-
 Can I get top surgery with other procedures like body masculinization or gender affirming body contouring?
Can I get top surgery with other procedures like body masculinization or gender affirming body contouring? -
Absolutely! Many of our patients opt for liposuction not only around their chest, but also around other parts of their body to alter their frame or silhouette. You can read more about the liposuction services we offer for the chest, back, flanks, abdomen, waist, hips, buttocks and thighs in our articles about body masculinization surgery and body contouring options for non-binary patients.
-
 How can I best prepare for top surgery?
How can I best prepare for top surgery? -
Prior to surgery, we recommend that patients work to maintain good physical and mental health. Minimizing or eliminating the consumption of alcohol and nicotine can also help ensure a positive surgical outcome. Learn more about our guidelines and recommendations here.
-
 Will top surgery change my level of chest and nipple sensation?
Will top surgery change my level of chest and nipple sensation? -
We offer many types of incisions and nipple reconstruction options that involve different levels of risk of sensation loss. Learn more about how top surgery can affect nipple sensitivity as well as the pain or soreness in mammary tissue caused by premenstrual syndrome here.
-
 How might top surgery impact breast cancer risk?
How might top surgery impact breast cancer risk? -
The risk that a top surgery patient has of acquiring breast cancer after surgery is largely dependent on how much tissue is removed along with their previous medical and family history. Read more about risk evaluation and best practices for breast cancer detection before and after surgery here.
-
 How might chest binding and nipple piercing affect top surgery results? When can I get my nipples pierced after surgery?
How might chest binding and nipple piercing affect top surgery results? When can I get my nipples pierced after surgery? -
Patients who previously used a chest binder and/or have had nipple piercings are still eligible for top surgery. The effects of chest binding on top surgery results are minimal at best. Still, long-term binding may affect skin elasticity. Please inform your surgeon if you had nipple piercings in the past. Any chest piercings will need to be removed prior to the operation. You can find more information on chest binding here, and our guidelines around nipple piercings here.
-
 How might top surgery and testosterone hormone replacement therapy (HRT) impact someone’s ability to get pregnant? How might pregnancy affect a patient’s top surgery results?
How might top surgery and testosterone hormone replacement therapy (HRT) impact someone’s ability to get pregnant? How might pregnancy affect a patient’s top surgery results? -
Though there is sparse medical research on the subject, many people who have been on testosterone hormone replacement therapy (HRT) and/or have had top surgery can still carry a pregnancy to term. There is evidence to suggest that some top surgery patients may experience mammary tissue growth during pregnancy. For more information about chestfeeding, HRT, top surgery and pregnancy, click here. For more specific questions, we recommend speaking with a trans or gender-competent medical provider. In the video below, Dr. Jacobs (he/him) addresses the unlikelihood that patients will be able to chest-feed after top surgery. Still, he mentions, there is a chance that the infant can bond with their parent’s chest even if they are incapable of milk production.
Top surgery encompasses a variety of mastectomy and breast reduction techniques as well as the possibility for liposuction. Here we go over every incision type our surgical center offers and why patients tend to opt for them:
- The double incision is ideal for patients with a large amount of chest/breast tissue and/or for those who desire as flat of a chest as possible. The nipple-sparing double incision is a similar procedure that can allow for greater preservation of nipple sensation.
- The periareolar incision is ideal for patients with moderate chest/breast tissue and appropriate skin elasticity. Incisions are made around the periphery of the areola so that scarring can be more discreet. The lollipop incision is a similar procedure that allows for additional skin to be removed to increase chest tightness.
- The inverted T and buttonhole incisions can be used for breast reductions or mastectomies. It leaves upside-down T or anchor shaped scars on the chest and is ideal for eliminating excess skin.
- The keyhole incision involves the creation of a small incision at the base of the areola to remove chest tissue. This procedure is ideal for patients with minimal mammary tissue, no loose skin and high skin elasticity.
- The fish mouth or batwing incision is one of our least common procedures. The incision placement can allow for the scar to appear more consistent with the border of the chest muscle; however, it involves the areolas being placed slightly higher than in their typical position.
If you would like to learn more about how we help patients determine which incision type, you can read more about the Mosser Method here. This method takes into account a patient’s inframammary angle, skin elasticity as well as goals around flatness and nipple sensation.
If interested, there are several alterations a patient can have us make to their areolas and nipples during top surgery. You can read more about the options we offer below to help determine which would be best for you:
-
 Nipple sparing/preservation: optimal to maintain heightened sensation
Nipple sparing/preservation: optimal to maintain heightened sensation -
Nipple sparing involves keeping the original nipple in-tact and attached to the pedicle: its original blood and nerve supply. This option has the highest probability of preserving heightened or erotic nipple sensation, though it often means complete chest flatness cannot be achieved. Read more about pedicle preservation in breast reductions here.
-
 Nipple grafting: optimal to control resizing and repositioning
Nipple grafting: optimal to control resizing and repositioning -
Nipple grafting is the most commonly selected option for top surgery patients. Grafting gives the surgeon the most control over repositioning and resizing the patient’s areolas and/or nipples. Likewise, this option is ideal for patients who wish to maximize chest flatness. However, grafting often results in patients losing heightened, erotic nipple sensation. Thanks to our surgeon’s high levels of experience, 98% of GCC’s nipple grafting is successful, meaning the grafted nipple survives the recovery process. This usually results in the nipple having the same level of sensation of the surrounding skin.
-
 No nipples or tattooed nipples
No nipples or tattooed nipples -
Some patients request that their nipples and areolas be removed from their chest during top surgery. The option to have no nipples is common in patients who wish to have a chest without them or who would prefer to have 3D, hyper realistic nipples tattooed onto their chest to avoid dealing with the recovery protocols and potential complications associated with nipple grafting.
We have put together a series of guides to cover the most common inquiries patients and their loved ones have about complications and recovery from top surgery. Every patient’s process is different. If you have inquiries about your unique situation or medical history, we can take that into account when crafting your unique surgical plan in a free, virtual consultation.
- For the general timeline for healing after surgery, click here
- For a guide on physical rehabilitation for pain and mobility, click here
- For guidelines on limiting arm movement post-op, click here
- For tips for speeding up the recovery process, click here
- For information on returning to work after surgery, click here
- For information on resuming exercise after surgery, click here
- For instructions on incision and scar care, click here
- For instructions on caring for nipple grafts, click here
- For information on surgical drains, click here
- For information on potential complications from top surgery, click here
Do you have specific questions about top surgery? You can get them answered and start the journey to getting top surgery by requesting a free, virtual consultation with one of our board-certified surgeons today.
Request a Free Surgical Consultation Today.
All virtual and in-person consultations with our board-certified surgeons are free. Once you fill out this form, our patient care team will reach out and guide you through every step to get to surgery.